Recovering from COVID-19
February 1stWith the sudden increase in COVID-19 infections within our community, our Kinematics team has created this as a resource for our clients to access to ensure you feel supported during your isolation, as well as empowered to make a full recovery.
As allied health practitioners, we play a key role in helping you recover from COVID-19, particularly by facilitating optimal functioning of both your cardio-respiratory and musculo-skeletal health. In order to give you the best chance at making a full recovery, it is important to address both of these body systems, as their functions are interconnected.
In this blog, we will provide insight alongside suggestions on how to manage some of the common signs and symptoms experienced with COVID-19.
We will cover:
-
Breathlessness
-
Coughing
-
Headaches
-
Fatigue
-
Pacing Activity
-
Exercise and Physical Activity
-
Returning to Work
1. BREATHLESSNESS
Being infected with coronavirus commonly results in an acute respiratory response. This can lead to compromised gas exchange within the linings of the lungs and therefore oxygen levels can dip and you may experience breathlessness.
You may notice that:
-
Your chest is tight
-
You find it difficult to catch your breath
-
You are breathing more quickly and using extra muscles to help
-
You might be panicky and anxious
-
You tire quickly
Shortness of breath can be quite frightening and therefore knowing how to control your breathing can help you remain calm. The below exercises can be used during activity or while you rest to help relieve shortness of breath, or to aid relaxation if you are feeling anxious.
For maximum relaxation during these breathing exercises, we suggest either sitting in a comfortable seated position or laying on your back with your head supported. Place one hand on your chest and the other hand on your belly for tactile feedback.
Breathing Exercises:
- Pursed-lips breathing: Breathe in through your nose, then out through your mouth with your lips pursed (like you are whistling). By using the pursed lip technique when breathing out, you create back pressure in the airways that stents the airway open longer. This helps to slow your breathing rate down and can help if you are feeling short of breath, fearful, anxious or stressed. Repeat at least five breath cycles.
- Box Breathing (4,4,4,4): Box breathing (also known as 4-squared breathing) is a type of paced breathing that follows a certain rhythm. This technique can help you to minimise stress and allow you to regain a comfortable breathing pattern. Begin the exercise by taking a deep breath in through your nose over a 4 second count followed by a hold for a 4 second count. Next, breathe out through your mouth over a 4 second count and hold for another 4 second count. Repeat for 10-15 rounds or as prescribed by your healthcare practitioner.
Positioning to reduce effort of breathing:
You can also try these different positions to reduce effort of breathing and help open and relax your airways.
- Lie on your back, with your legs rested on a box or bench.

- Sit down and lean forward. Rest both arms on either your thighs or a table/bench. Relax your hands and wrists.

- Positions for resting and sleeping: You may find it helpful to try sleeping on your front or side with pillows for support. This will avoid the effect of gravity that places extra pressure on your chest and lungs, and it will assist with drainage of any fluid in the chest.
While these exercises can be effective at reducing breathlessness and anxiety, you should seek urgent medical help if you have severe shortness of breath, are suddenly confused or your lips or face are turning blue.
2. COUGHING
Coughing is the body’s way of protecting our lungs and getting rid of things that irritate them. Following a respiratory infection we can be left with a dry cough because our lungs have been irritated. It can be difficult to control your cough, however there are a few techniques which may help.
If you have a dry and irritable cough, taking regular sips of water may help to reduce the frequency of your coughing. You can also consider using some of the positions suggested above to reduce your effort of breathing.
If you have a productive cough, we recommend trying the Active cycle of breathing technique (ACBT). The ACBT combines different breathing techniques that help clear mucus from the lungs in three phases. The first phase (breathing control) helps you relax your airways. The second phase (deep breathing) helps you to get air behind mucus and clears mucus. The third phase (huffing) helps force the mucus out of your lungs.
Breathing control: Breathing control is breathing gently, using very little effort. Breathe in through your nose and out through your mouth. Focus on letting go of any tension in your body with each breath out and gradually try to make these breaths slower. You can also close your eyes to help you relax and bring focus to your breath. Complete 20-30 seconds.
Deep breathing: Take a long, slow, deep breath in through your nose and think of filling up the base of your lungs by expanding your ribs outwards. Try to keep your chest and shoulders relaxed. Breathe out gently and relaxed (like a sigh). Complete 3-5 deep breaths.
**Repeat two cycles of breathing control + deep breathing before huffing (as per diagram)**
Huffing: A huff is a breath out (exhalation) through an open mouth and throat that helps move mucus up your airways so that you can clear it in a controlled way. It is different to a cough as it allows your airways to stay open as the sputum moves its way up and out. To huff, squeeze air quickly out of your lungs like you’re fogging up a mirror with your breath. You can hold your hand up in front of your mouth to help reproduce this action. Use your tummy muscles to help you squeeze the air out, but do not force it so much that you cause wheezing or tightness in your chest. Huffing should always be followed by another round of breathing control.
3. HEADACHE
Another common symptom of COVID-19 that we have also seen is unrelenting headaches. Headaches may be caused by a number of different reasons including dehydration, lack of sleep or muscle tension. Here are some techniques to help self manage some of the tension that you may be feeling in your head. Whilst doing these techniques, remember to focus on your deep breathing.
-
Facial release 1 (sinus): Using your index finger, gently apply pressure either side of your nose. Start with making small circular motions (3-4x), then swipe in an outwards motion along your cheekbone towards your ear. Repeat 3-5 times.
-
Facial release 2 (temple): Using 2-3 fingers, gently apply pressure to your temples and move in a circular motion. Continue massaging for 30 seconds.
-
Facial release 3 (sinus): Using your index finger, gently apply pressure to the base of your eyebrows (near the bridge of your nose). Swipe in an outwards motion along your eyebrow towards your ear. Repeat 3-5 times.
If your headaches persist and don’t seem to be getting better, please don’t hesitate to get advice from your GP or allied health care professional.
4. FATIGUE
Fatigue is commonly experienced with COVID-19 and is most likely a consequence of the rapid multiplication and spread of the virus in the body, which slows down functions.
Here are some tips to help manage your fatigue:
-
Plan how you will do your activities before starting to avoid wasting energy. For example, gather toiletries and towels before walking to the bathroom to save multiple trips.
-
Plan your activities for when you feel less tired. For example, you might feel better in the morning rather than the afternoon.
-
Spread out tasks throughout the day, take regular breaks and have a short nap if you need it.
-
Give yourself plenty of time to do activities.
-
Don’t be too hard on yourself and accept that some days will be better than others.
-
Sleeping well can help you feel less tired and can also help with your recovery and healing.
-
Have a period of ‘downtime’ before bed. Limit your use of devices such as phones and tablets, to minimise light and noise.
You may not feel like doing any physical activity, however, regular movement can give you more energy and make you feel less fatigue in the long run.
Try these gentle exercises to keep you mobile while you are in isolation and help gradually reintroduce your body to physical activity.
Cobras:
- This exercise is great for mobilising the mid back which can get very stiff after a period of immobility.
- Progress by adding in variations.
- For all variations maintain a neutral chin and progress the back extension height as able.
- Repeat each variation x15 twice a day
VARIATIONS:
Cobra 1 (active assisted with arms): Begin laying on your stomach with your arms underneath your armpits. Set your shoulders back, tense your glutes and press through your arms to lift your chest off of the ground. Keep your chin in neutral and elbows touching your side. The main focus of this exercise is to extend through the thoracic spine (upper back), so you shouldn’t feel any pinching in your lower back (if you do, first try exaggerating the glute squeeze and not lifting your chest as high).
Cobra 2 (unassisted): Begin laying on your stomach with your arms underneath your armpits. Lift your hands off of the ground. Set your shoulders back, tense your glutes and then lift your hands off of the ground. Then begin the chest lift with no assistance from your arms.
Cobra 3 (active assisted with foam roller): Begin laying on your stomach with your arms above your head. Place your wrists on a foam roller with thumbs facing towards the ceiling, just outside of shoulder width. Pull your shoulders down and away from your ears, tense your glutes, and press down into the roller as you begin to lift your chest off of the ground.
Child’s pose + side bend stretch
- x10-15 reps, twice a day.
- This exercise stretches out the posterior and lateral trunk which commonly becomes tight if breathing is shallow and movement is limited.
-
To begin the exercise, sit on your heels with your knees apart and arms stretched out overhead. Take a deep breath in through your nose. As you breath out start to press your chest through your shoulders and extend through the thoracic spine. Rock in and out of the stretch by shifting your body weight forward onto your hands. To achieve a greater stretch lift up onto your fingertips to allow your chest to sink lower. To bias one side of the trunk, walk your hands to the left and then the right.
Chest + Thoracic Mobility
- x10-15 reps, twice a day.
- This exercise stretches out the anterior chest and mobilises the thoracic spine which commonly becomes tight if breathing is shallow and movement is limited.
- Start in a half kneeling position with your front leg against the wall. If you struggle to kneel on your knees without pain, be sure to place a piece of foam or pillow under under your knee. Next, tuck your tailbone by squeezing your glutes on. With your palm facing the wall, begin to windmill the arm overhead. Limit any compensations by not letting yourself push away from or rotate towards the wall. Follow this with a thoracic rotation. As you rotate, make sure your hips don’t follow your trunk and you lead the rotation from your ribcage. The goal is to get the back of your shoulder to touch the wall.
5. PACING ACTIVITY
It is important to listen to your body and gradually return to normal activity after a period of illness. It can be very frustrating as your mind may feel that you should be able to do more than your body allows you to. Remember, activity can be both physically and mentally tasking.
Pacing lets you plan out your activity and rest periods over the course of the day which will allow you to gradually increase your activity. Simply add activities you have completed during the day and think about a possible plan for tomorrow. You can also use this to look back and see how you have progressed during your recovery.
6. EXERCISE + PHYSICAL ACTIVITY
It is beneficial to return to physical activity as soon as possible, to maintain cardiovascular health and musculoskeletal strength (even if it is gentle to begin with).
If your walking is limited, do as much as you feel able. Walking short distances regularly in the house is better than sitting for long periods. Little and often is key.
For example:
-
Start by walking for around five to ten minutes at a comfortable pace, and aim to increase this by a couple of minutes each day. You should not feel too breathless and be able to chat and regain control of your breathing while walking. It is normal to feel tired after any activity but you should not still feel tired the next day.
-
Use stairs to introduce some difficulty.
-
Try starting with isometric strength exercise and aim for longer holds rather than higher sets. Isometric exercises fatigue isolated muscle groups without a huge aerobic demand.
Below is a table outlining a gradual return to vigourous physical activity from early stages of illness.
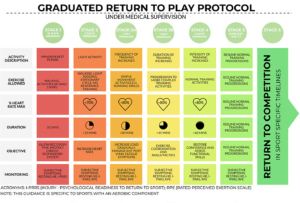
Source: BJSM Graduated return to play guidance following COVID-19 infection, 2020.
7. RETURNING TO WORK
A phased return to work is recommended wherever possible. This means that you gradually build up your hours and days, with lighter duties as appropriate. An appropriate return to work strategy can be discussed with your manager, GP and/or allied health professional.
Do not be surprised if you find yourself tired when you return to work. Just as being unwell is very individual, recovery is also very individual so keep in mind how you feel physically and mentally upon your return to your workplace.
Having good postural mobility is key in helping to get through a working day without feeling sore, tight or fatigued, especially if we are in a job that involves sitting for long periods. We recommend continuing the home mobility exercises demonstrated above (in section 4. Fatigue) to minimise the effects of prolonged sitting on your posture.

We hope that you feel encouraged by the many ways in which you can help manage your symptoms, and ultimately contribute to regaining your full health.
The Kinematics team would love to help support you to make a full recovery from COVID-19. You can either contact the reception team to make a telehealth appointment, or alternatively once you’ve completed your isolation period, you can book in to see one of our team here.
By Jonathan Covich, Elise McMahon and Amy Wiley
Physiotherapists | Kinematics Health + Performance